Sponsored by Medtronic
By Tim Nowak for EMS1 BrandFocus
COVID-19 has changed some of what we do in our line of work, especially when it comes to airway management procedures for respiratory distress and failure patients (and that may be a bit of an under-statement, to say the least).

Nevertheless, these changes have raised concerns over what types of advanced airways should be utilized, what barrier devices should be placed inline to prevent contamination spread, and whether or not our expensive monitoring equipment will become contaminated as a result of exhaled gas intake for sampling purposes, particularly with end-tidal carbon dioxide (EtCO2) sampling.
Well, rest assured that the answer here is no – you’re not doing anything wrong by continuing to monitor EtCO2 values. In fact, safeguards have been in place long before COVID-19 even hit the spotlight, and you’re doing the right thing by continuing to monitor EtCO2 values and capnograph waveforms. These assessments remain the gold standard for airway/respiratory evaluations.
Moreover, your sampling capno-cannulas and inline airway device adapters are doing more to protect you and your patient (and your equipment) than you’re probably aware. For instance, standard N95 masks have a filtering property of stopping particles as small as 0.3 microns in size. In comparison, the filter present in the Microstream sampling lines from Medtronic can block particles as small as 0.2 microns in size. This means fluids, bacteria and viruses are filtered out prior to entering any monitor.
Challenges can still arise with respect to airway/respiratory patient assessment, but your level of safety shouldn’t be compromised as a result of these challenges. In fact, let’s break some of them down right now.
Decreasing SpO2 Values
This is almost a trick question, because capnographs don’t measure oxygen (O2) values – they measure carbon dioxide (CO2) values – but this isn’t exactly the point. Where the point rests here is with their assessment correlation. COVID-19 patients often present as patients that maintain adequate-to-low SpO2 values ... until they don’t ... and that downturn can occur rapidly. EtCO2 values, however, remain accurate and reflective of a patient’s ventilatory and metabolic/perfusion status, regardless of their SpO2 values.
Order of Connection
As a good rule of thumb, always keep your EtCO2 adapter connected as close to your advanced airway device – or CPAP mask – as possible. Hindering sampling airflow with tube extensions, HEPA filters and other adapters can cause a decreased sampling size to be obtained for adequate assessment. As such, always keep your adapter connected as close to the patient as possible.
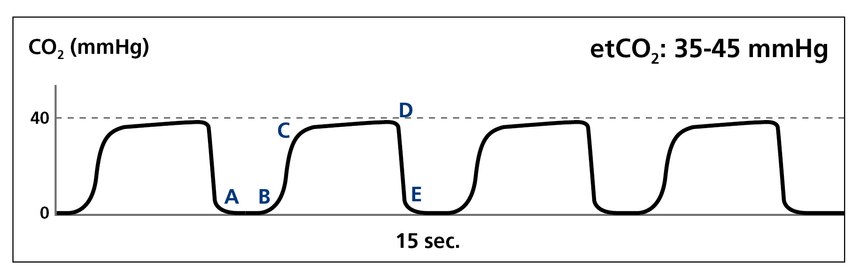
Waveforms Remain the Same
Interpretation of capnograph waveforms remains the same with COVID-19 patients as with any other patient. There isn’t a fancy COVID-wave like you envision with bronchospasmatic “shark fin” waveforms (although that would be interesting). Obstruction still means obstruction, and bronchospasm still means bronchospasm.
COVID Doesn’t Change Things , But It Can Complicate THEM
Think about a sepsis patient for a moment. Tachycardia, hyperthermia, tachypnea, hypotension, infection and hypocapnia are all classic signs of sepsis, and they’re also possible indicators of COVID-19. The point in highlighting this is that COVID-19 doesn’t necessarily change anything about any number of existing/prior disease processes, but it sure can complicate them! Use your best clinical judgment to determine patient treatment, and of course, reference your local clinical protocols.
Clean as Recommended
Capnography consumables are a disposable item. Refer to the manufacturer’s recommendations for your monitors for cleaning and wipe down, and follow current CDC guidelines.
Overall, keep doing what you’re doing. Keep caring for your patients, keep transporting sick and injured patients, and keep following the most up-to-date recommendations being rolled out by your administrative and leadership team with respect to patient care protocols.
And, rest assured that when it comes to EtCO2 monitoring, you’re (still) doing the right thing!
Visit Medtronic for more information.
Read Next: Troubleshooting common capnography challenges: 3 tips for better results
"right" - Google News
October 16, 2020 at 10:40PM
https://ift.tt/37exwwz
EtCO2 monitoring: You're doing the right thing - EMS1.com
"right" - Google News
https://ift.tt/32Okh02
Bagikan Berita Ini














0 Response to "EtCO2 monitoring: You're doing the right thing - EMS1.com"
Post a Comment